Annotation Guidelines
This page gives an overview of the annotation and normalization scheme and process of the SympTEMIST corpus. More detailed information is available in the Annotation Guidelines, which document the corpus’ creation and annotation process. They are available on Zenodo.
The SympTEMIST guidelines were created by clinical experts concurrently with the DisTEMIST and ProcTEMIST guidelines. Just as with the mentioned corpora, the guidelines were refined in several cycles of quality control and annotation consistency analysis before annotating the entire dataset. Additionally, once the manual annotation phase was finished, the corpus was thoroughly revised in a post-processing step to maximize consistency.
The corpus includes only one label: SINTOMA (symptom). Despite the name, the label covers signs, symptoms and findings, making the information within it quite varied in form and content. Some specific examples are:
- Signs and symptoms: health-related problems expressed by the patient (“pain in left lower limb”, “(they) hear voices”) or found by a doctor during examination (“disoriented”, “increased peristalsis”).
- Test results: non-numerical descriptions of test results (“elevated white blood cell”) and general procedures, including mentions of normality (“no ECG abnormalities”).
- Imaging procedures: descriptions of static and dynamic imaging procedures (“dilated right atrium”, “crazy-paving pattern”). This does not include diagnoses, which are covered by DisTEMIST.
- Patient death: “died”, “passed away”.
These are some screenshots of the corpus content shown in brat:

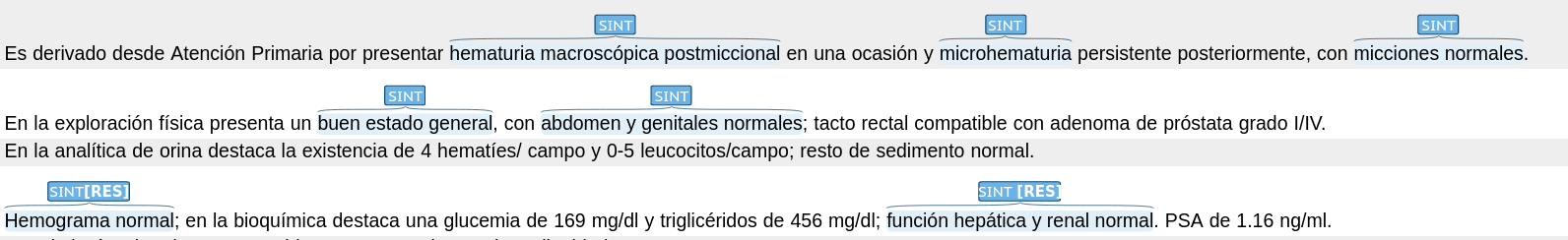
He was referred from Primary Care for presenting gross hematuria on one occasion and persistent microhematuria later, with normal micturition.
Physical examination showed a good general condition, with normal abdomen and genitalia; rectal examination compatible with grade I/IV prostate adenoma.
Urinalysis showed 4 red blood cells/field and 0-5 leukocytes/field; the rest of the sediment was normal.
Normal hemogram; the biochemistry shows a blood glucose of 169 mg/dl and triglycerides of 456 mg/dl; normal hepatic and renal function. PSA of 1.16 ng/ml.

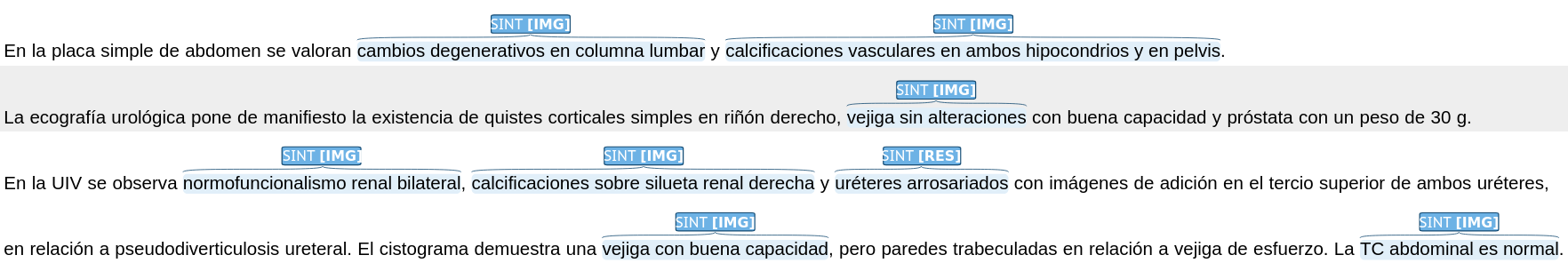
The simple abdominal x-ray shows degenerative changes in the lumbar spine and vascular calcifications in both hypochondrium and pelvis.
The urological ultrasound revealed the existence of simple cortical cysts in the right kidney, bladder without alterations with good capacity and prostate weighing 30g.
IVUS shows bilateral renal normofunctionalism, calcifications on the right renal silhouette and arthrosed ureters with addition images in the upper third of both ureters, related to ureteral pseudodiverticulosis. The cystogram shows a bladder with good capacity, but trabeculated walls in relation to stress bladder. The abdominal CT scan is normal.

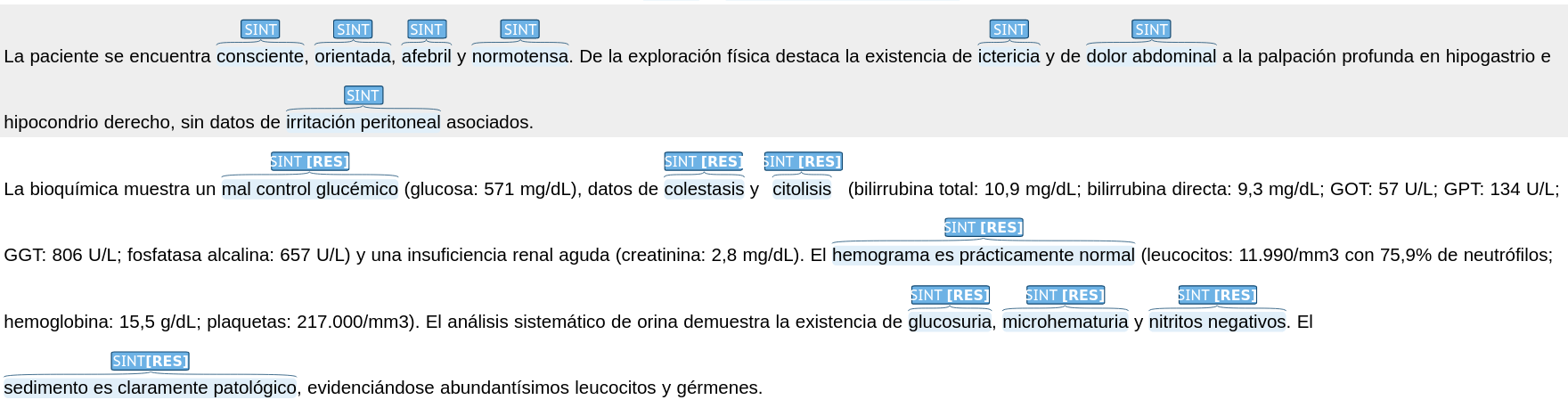
The patient was conscious, oriented, afebrile and normotensive. Physical examination revealed jaundice and abdominal pain on deep palpation in the hypogastrium and right hypochondrium, with no associated peritoneal irritation.
Biochemistry shows poor glycemic control (glucose: 571 mg/dL), cholestasis and cytolysis (total bilirubin: 10.9 mg/dL; direct bilirubin: 9.3 mg/dL; GOT: 57 U/L; GPT: 134 U/L; GGT: 806 U/L; alkaline phosphatase: 657 U/L) and acute renal failure (creatinine: 2.8 mg/dL). The hemogram is practically normal (leukocytes: 11,990/mm3 with 75.9% neutrophils; hemoglobin: 15.5 g/dL; platelets: 217,000/mm3). Systematic urinalysis shows glycosuria, microhematuria and negative nitrites. The sediment is clearly pathological, showing abundant leukocytes and germs.

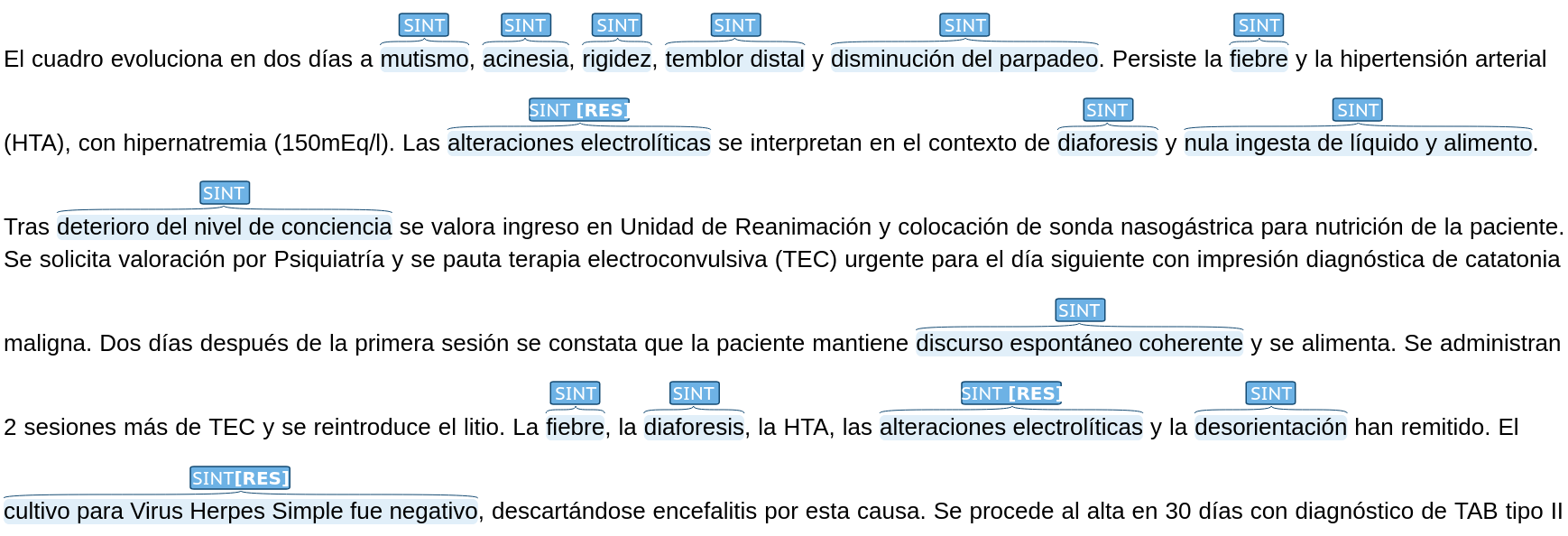
The condition evolves in two days to mutism, akinesia, rigidity, distal tremor and decreased blinking. Fever and arterial hypertension persist, with hypernatremia (150mEq/l). Electrolyte disturbances are interpreted in the context of diaphoresis and no fluid and food intake. After deterioration of the level of consciousness, admission to the Resuscitation Unit and placement of a nasogastric tube for nutrition of the patient was assessed. Psychiatric evaluation was requested and electroconvulsive therapy (ECT) was prescribed urgently for the following day with the diagnostic impression of malignant catatonia. Two days after the first session, the patient was found to have coherent spontaneous speech and was eating. Two more sessions of ECT were administered and lithium was reintroduced. Fever, diaphoresis, hypertension, electrolyte disturbances and disorientation have subsided. The culture for Herpes Simplex Virus was negative, ruling out encephalitis due to this cause. [...]

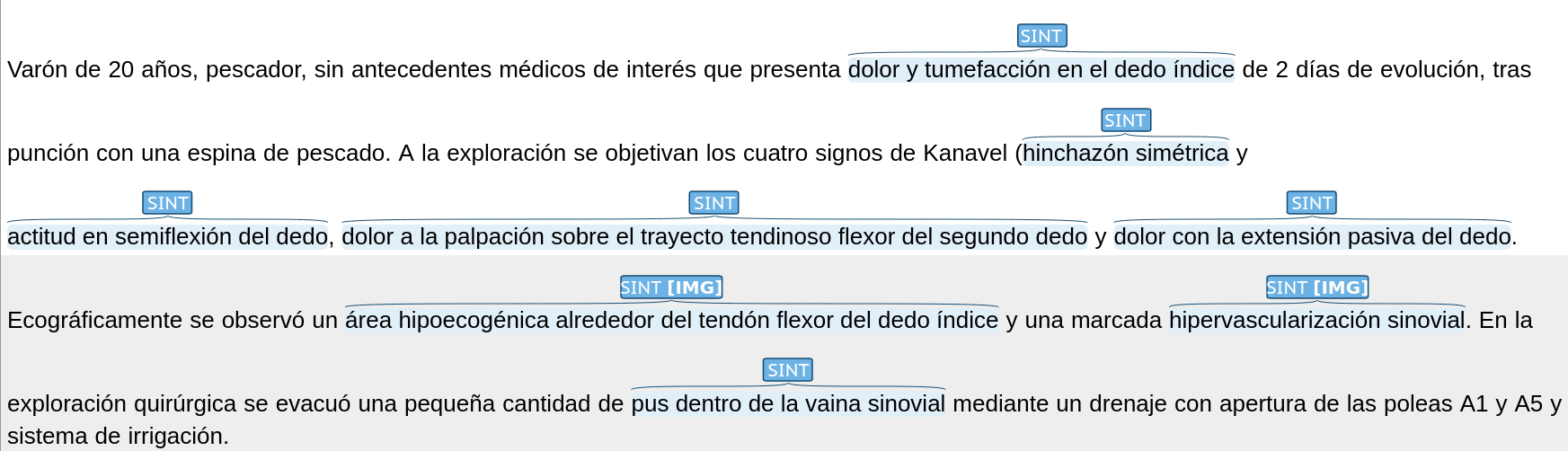
A 20-year-old male fisherman with no medical history of interest presented with pain and swelling in the index finger of 2 days' evolution, after puncture with a fish bone. On examination, the four Kanavel signs were observed (symmetrical swelling and semi-flexed attitude of the finger, pain on palpation over the flexor tendon path of the second finger and pain with passive extension of the finger).
The ultrasound revealed a hypoechogenic area around the flexor tendon of the index finger and marked synovial hypervascularization. On surgical exploration, a small amount of pus within the synovial sheath was evacuated by drainage with opening of the A1 and A5 pulleys and irrigation system.